
Many with endometrial cancer will not have any of these symptoms. Some may only report light spotting. This is an important sign and needs to be discussed with your physician.
If endometrial cancer is suspected, the tests and procedures used to diagnose endometrial cancer include the following:
1 . Imaging to visualize the uterus and other pelvic structures to assess for abnormalities. They can also show if and how far the cancer has spread beyond the uterus. This may include an ultrasound, CT scan, PET scan or MRI.

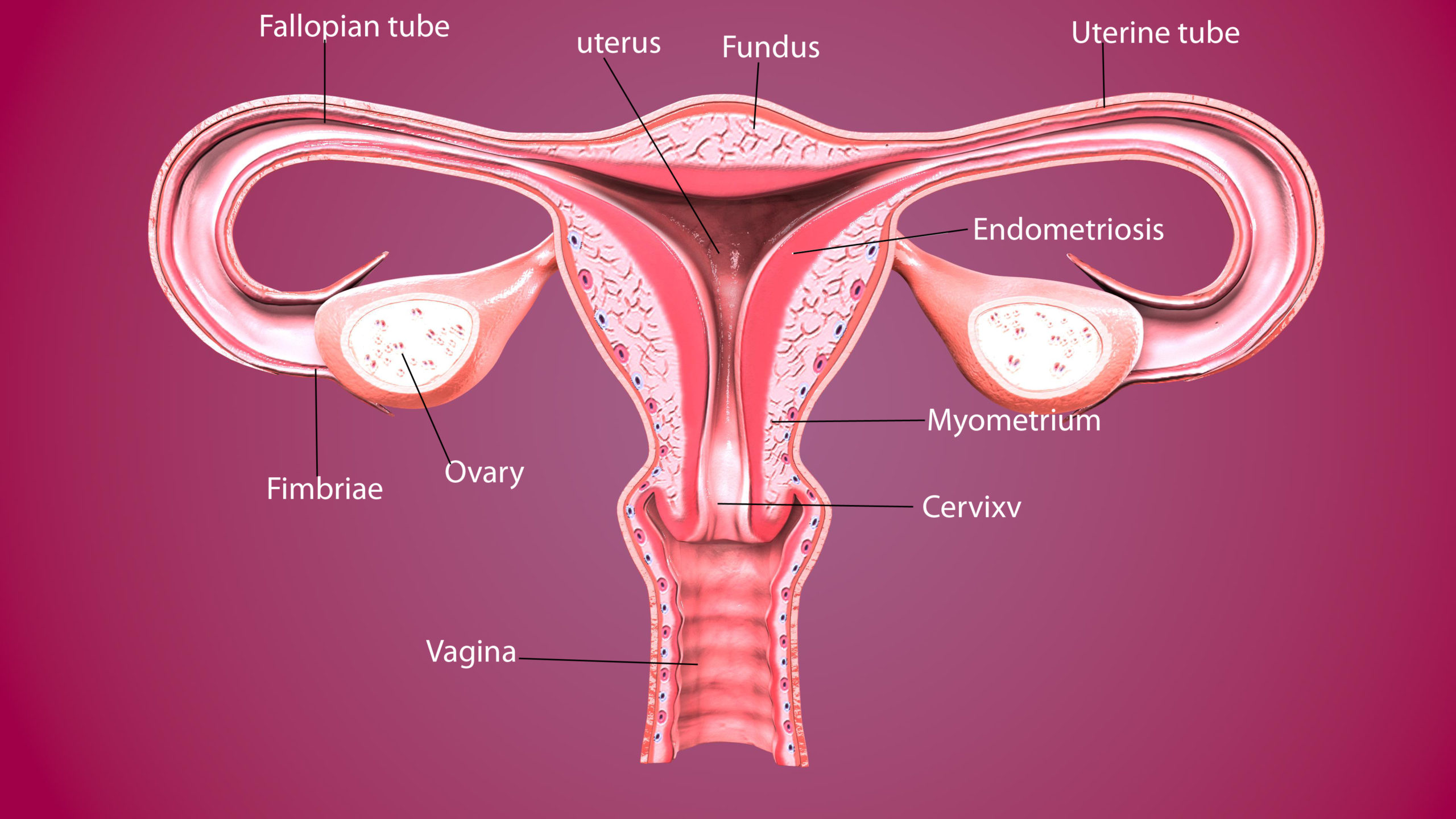
2. Endometrial biopsy – Endometrial cancer begins inside the uterus and does not show up on a pap smear. For this reason, an endometrial biopsy is done by passing a thin, flexible tube through the cervix into the uterus. The biopsy is then sent to pathology. Sometimes this biopsy is not possible or results in insufficient sampling, in which further testing is needed.
3. Hysteroscopy – A procedure to look inside the uterus for abnormalities.
4. D&C – (dilation and curettage) usually done in addition to a hysteroscopy, is a procedure done under anesthesia to remove a larger amount of tissue from the inner lining of the uterus.


Staging can be complex and further explanation will be provided by your physician.
| Stage | Stage description* |
| I | The cancer is growing inside the uterus. It may also be growing into the glands of the cervix, but not into the supporting connective tissue of the cervix.
It has not spread to nearby lymph nodes or to distant sites. |
| IA | The cancer is in the endometrium (inner lining of the uterus) and may have grown less than halfway through the underlying muscle layer of the uterus (the myometrium) (T1a).
It has not spread to nearby lymph nodes or to distant sites. |
| IB | The cancer has grown from the endometrium into the myometrium. It has grown more than halfway through the myometrium, but has not spread beyond the body of the uterus .
It has not spread to nearby lymph nodes or to distant sites. |
| II
|
The cancer has spread from the body of the uterus and is growing into the supporting connective tissue of the cervix (called the cervical stroma). But it has not spread outside the uterus.
It has not spread to nearby lymph nodes or to distant sites. |
| III | The cancer has spread outside the uterus, but has not spread to the inner lining of the rectum or urinary bladder.
It has not spread to nearby lymph nodes or to distant sites |
| IIIA | The cancer has spread to the outer surface of the uterus (called the serosa) and/or to the fallopian tubes or ovaries (the adnexa)
It has not spread to nearby lymph nodes or to distant sites |
| IIIB | The cancer has spread to the vagina or to the tissues around the uterus (the parametrium)
It has not spread to nearby lymph nodes (N0) or to distant sites |
| IIIC1 | The cancer is growing in the body of the uterus. It may have spread to some nearby tissues, but is not growing into the inside of the bladder or rectum
It has also spread to pelvic lymph nodes, but not to lymph nodes around the aorta or distant sites. |
| IIIC2 | The cancer is growing in the body of the uterus. It may have spread to some nearby tissues, but is not growing into the inside of the bladder or rectum.
It has also spread to lymph nodes around the aorta (para-aortic lymph nodes) but not to distant sites |
| IVA | The cancer has spread to the inner lining of the rectum or urinary bladder (called the mucosa)
It may or may not have spread to nearby lymph nodes, but has not spread to distant sites |
| IVB | The cancer has spread to inguinal (groin) lymph nodes, the upper abdomen, the omentum, or to organs away from the uterus, such as the lungs, liver, or bones.
The cancer can be any size and it might or might not have spread to other lymph nodes. |
For more information on Endometrial Cancer Stages:
https://www.cancer.org/cancer/endometrial-cancer/detection-diagnosis-staging/staging.html