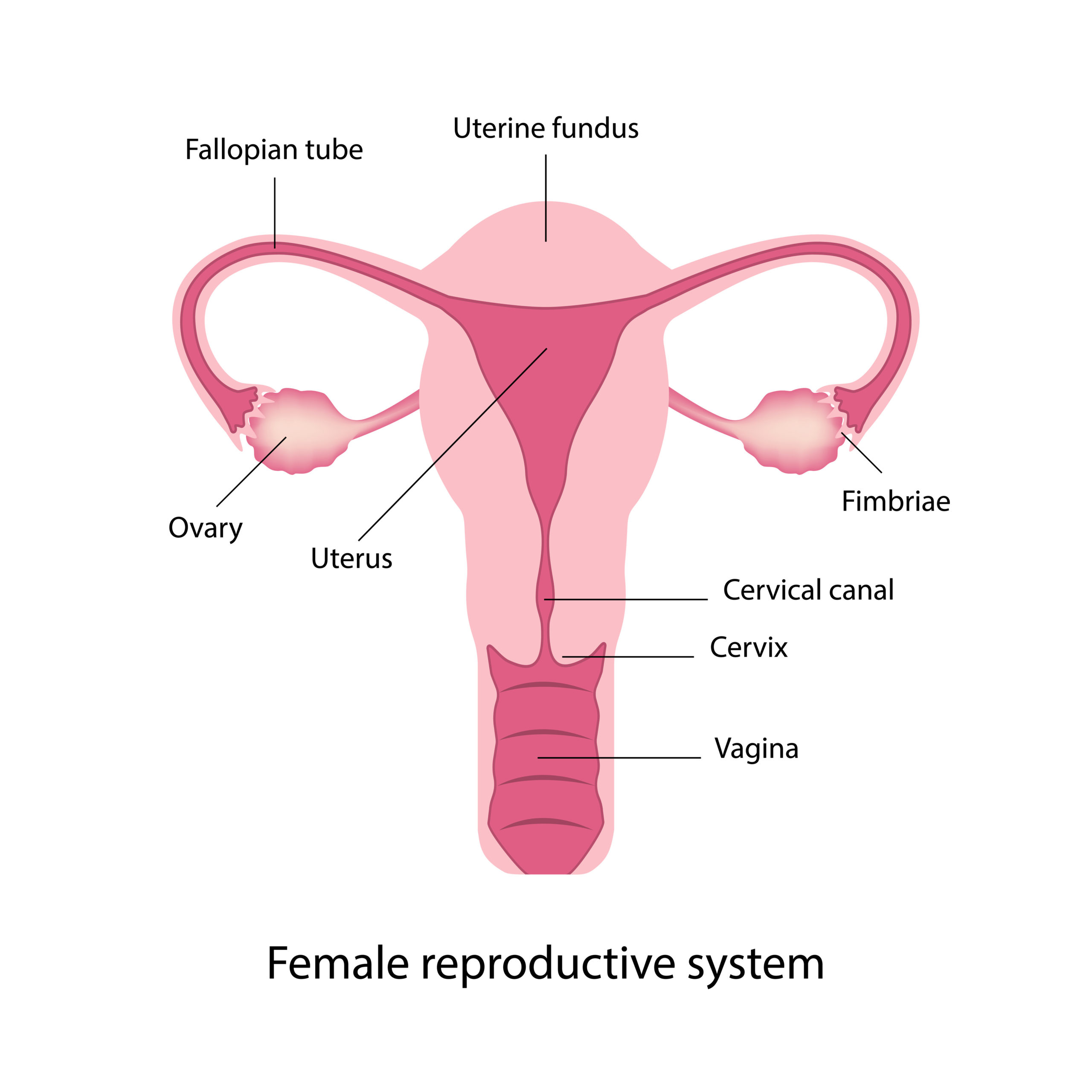
The vagina is an elastic, muscular canal with a flexible lining that provides lubrication and sensation. The vaginal canal connects the uterus and cervix to the outside world as the cervix protrudes into the vagina. During childbirth, the baby passes through the vagina, also known as the birth canal. The vaginal canal also allows for menstruation and intercourse.
HPV (Human papillomavirus) is the most common sexually transmitted infection and the most common cause of vaginal cancer. Having a history of cervical/vaginal dysplasia is associated with an increased risk for vaginal cancer. Vaginal cancer can occur before or after a hysterectomy. This is why having vaginal pap smears after a hysterectomy is even more important if you have a history of HPV.
Risk factors:
Early-stage vaginal cancer generally produces no symptoms.

Signs and symptoms of more advanced vaginal cancer include:
Vaginal cancer is usually preventable with routine pelvic exams and pap smears, HPV screening and the HPV vaccine.
This is why close monitoring with pap smears and routine pelvic exams, even after a hysterectomy, is important. A pap smear is a test to sample cells on the surface of the cervix and can be done on the vaginal as well to screen for vaginal dysplasia/Vaginal cancer. HPV testing can be done at the same time.

Although a pap smear can identify vaginal dysplasia, further tests are often required. If you have had an abnormal pap or exam findings a treatment/monitoring plan will be individualized and determined by your physician.
Diagnosis:
Treatment options for vaginal cancer will be individualized and based on physical exam pathology results and imaging. Treatment may include:

Ways you can reduce your risk of developing vaginal cancer:
Staging is based on:
Staging can be complex and further explanation will be provided by your physician.
| Stage | Stage description* |
| IA | The cancer is only in the vagina and is no larger than 2 cm (4/5 inch)
It has not spread to nearby lymph nodes or to distant sites. |
| IB | The cancer is only in the vagina and is larger than 2.0 cm (4/5 inch)
It has not spread to nearby lymph nodes or to distant sites. |
| IIA | The cancer has grown through the vaginal wall, but not as far as the pelvic wall and is no larger than 2.0 cm (4/5 inch)
It has not spread to nearby lymph nodes or to distant sites |
| IIB | The cancer has grown through the vaginal wall, but not as far as the pelvic wall and is larger than 2.0 cm (4/5 inch)
It has not spread to nearby lymph nodes or to distant sites. |
| III | The cancer can be any size and might be growing into the pelvic wall and/or has blocked the flow of urine (hydronephrosis) which is causing the kidneys to not work.
It has also spread to nearby lymph nodes in the pelvis or groin (inguinal) area but not distant sites. |
| III | The cancer is growing into the pelvic wall and/or has blocked the flow of urine (hydronephrosis) which is causing the kidneys to not work.
It has not spread to nearby lymph nodes or to distant sites |
| IVA | The cancer is growing into the bladder or rectum or is growing out of the pelvis.
It might or might not have spread to lymph nodes in the pelvis or groin (inguinal area) It has not spread to distant sites. |
| IVB | The cancer has spread to distant organs such as the lungs, liver, or bones. It can be any size and might or might not have grown into nearby structures or organs.
It might or might not have spread to nearby lymph nodes. |
For more information on Vaginal Cancer:
https://www.cancer.org/cancer/vaginal-cancer/detection-diagnosis-staging/staging.html